6 Simple Steps to Heal Anal Fistula Faster in 2025
- April 19, 2025
Introduction
Anal fistulas can cause significant pain and discomfort, affecting many people.. An anal fistula is an abnormal connection between the skin near the anus and the anal canal, often resulting from an infection in an anal gland. The healing process can be lengthy, especially if not managed properly. However, with the right fistula treatment in Ayurveda and care, healing can be expedited significantly. Kshar Sutra treatment, known for its effectiveness, has been proven to speed up recovery for many patients. In this article, we’ll walk you through 6 simple steps to heal anal fistula faster in 2025 for a speedy recovery.
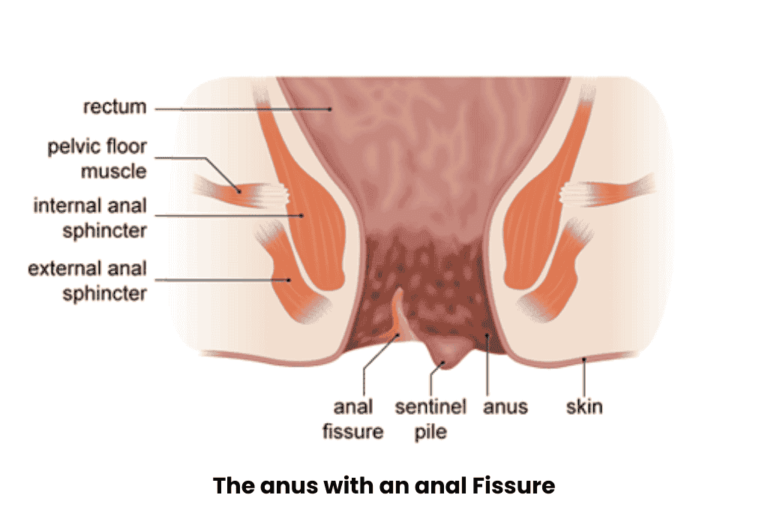
What is Anal Fistula?
An anal fistula is a small tunnel that connects an infected gland inside the anus to the skin outside. It typically develops after an anal abscess, which is a painful swollen area that forms from an infection. When the abscess does not heal completely, a fistula may develop. Some common symptoms of anal fistula include:
- Pain and swelling near the anus
- Discharge or bleeding from the opening near the anus
- Irritation or itching around the anal area
- Discomfort while sitting or during bowel movements
While the condition can be uncomfortable, it is treatable with the right approach, especially when diagnosed early. Fistula treatment in Ayurveda can be a holistic option for managing symptoms effectively.
Here are 6 Simple Steps to Heal Anal Fistula Faster
These 6 simple yet effective steps to accelerate the healing of anal fistulas. Follow these tips to ensure a quicker and smoother recovery process.
Ideal for patients with simpler fistula cases, this treatment offers a quick and effective solution with minimal discomfort.
1. Follow Your Doctor's Recommendations
The most important step is to follow your doctor’s advice to ensure quick healing. Dr. S.K. Singh, one of the best proctologists in Delhi, emphasizes the following:
- Regular check-ups: Regular visits to your doctor will help track your progress and prevent complications.
- Medications and treatments: Follow the prescribed treatments to promote healing.
- Early detection: Early identification of any issues can prevent delays in healing and ensure a smooth recovery.
Laser therapy is an excellent choice for patients seeking an effective, fast-acting, and minimally invasive solution for their anal fistula treatment.
2. Opt for Non-Surgical Treatment Options

Non-surgical treatments are less invasive and come with faster recovery times. Consider these effective options:
- Kshar Sutra Treatment: This is a minimally invasive treatment where a medicated thread is placed inside the fistula to clean and heal the tract. It’s a proven method that promotes faster anal fistula recovery.
- Ayurvedic Treatment: Herbs like turmeric and Triphala are known for their healing properties and can support the body in reducing inflammation, thereby aiding fistula healing.
- Fibrin Glue: A glue-like substance is injected into the fistula to seal it and promote healing without surgery.
- Seton Placement: A flexible material that drains the fistula, helping it heal naturally. It’s a great option for more complex cases.
This treatment is best suited for patients with complex anal fistulas that require a more long-term and reliable solution.
3. Maintain Proper Hygiene

Good hygiene is crucial for healing and preventing infections. Follow these tips:
- Gentle washing: Clean the anal area gently with warm water after bowel movements.
- Avoid harsh products: Don’t use strong soaps or chemicals that can irritate the skin.
- Pat dry: Always gently pat the area dry with a soft towel after washing to avoid further irritation and promote fistula healing.
- Use wet wipes: Wet wipes can be more soothing than dry toilet paper, minimizing irritation during cleaning.
Good hygiene habits play a critical role in speeding up anal fistula recovery and preventing future infections.
4. Eat a High-Fiber Diet

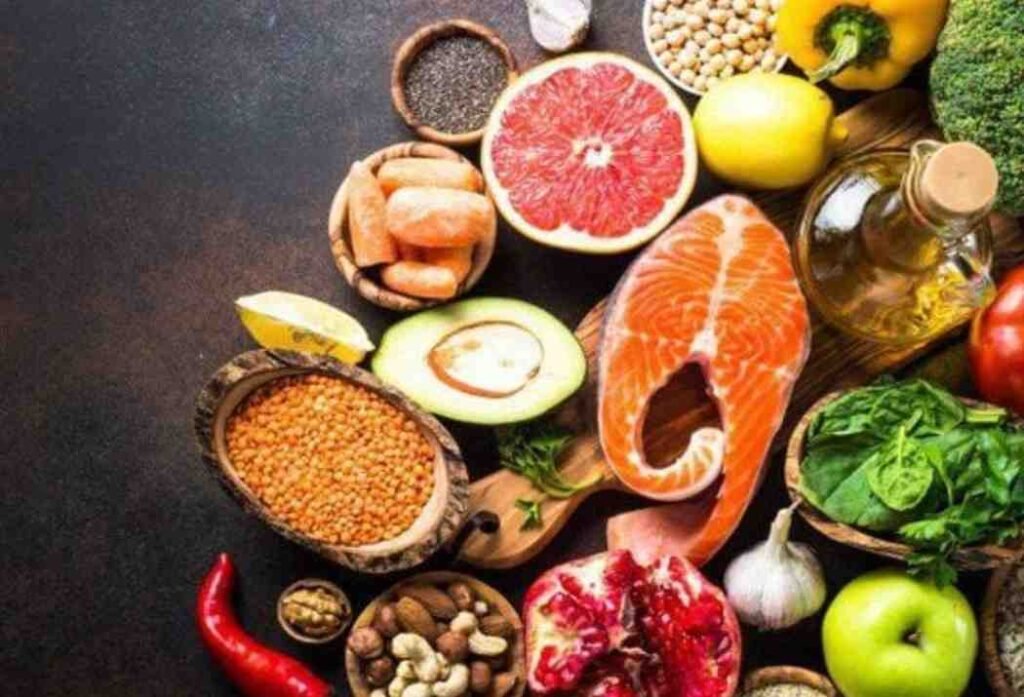
A proper diet helps make bowel movements easier and prevents strain. Here’s what you can do:
- Increase fiber intake: Foods like fruits, vegetables, and whole grains help soften stool, which makes bowel movements easier and less painful during anal fistula recovery.
- Stay hydrated: Drink plenty of water throughout the day to prevent constipation and ensure healthy digestion, both of which are important for fistula healing.
- Avoid spicy foods: Spicy foods can irritate the digestive system and slow down the healing process. It’s better to stick with gentle, soothing foods that support overall wellness.
A proper diet is integral to anal fistula treatment and improving recovery outcomes.
5. Avoid Straining During Bowel Movements

Straining during bowel movements puts extra pressure on the fistula and can slow healing. To avoid this:
- Use stool softeners: Stool softeners help prevent straining and make bowel movements smoother.
- Maintain a regular bathroom routine: Try to go to the bathroom at the same time each day to avoid rushing.
- Avoid sitting too long: Don’t sit for long periods on the toilet as it puts pressure on the affected area.
By following these steps, you can support your anal fistula recovery and reduce discomfort during fistula healing.
6. Get Enough Rest

Rest is essential for the body’s healing process. Follow these tips for optimal rest:
- Avoid long sitting periods: Sitting for long hours can increase pressure on the anal area. Use a cushion or doughnut-shaped pillow if necessary.
- Get enough sleep: Aim for 7-8 hours of quality sleep each night to help your body heal and repair tissues.
Rest is key to speeding up recovery and reducing stress.
What to Avoid During Recovery
During the recovery phase, certain activities or habits should be avoided to ensure a speedy healing process. These include:
- Avoid sitting for extended periods: This can put additional pressure on the fistula and slow down healing. It’s essential to avoid prolonged sitting to speed up the fistula healing process.
- Don’t engage in strenuous physical activity: Lifting heavy objects or engaging in vigorous exercise can place strain on the affected area, hindering anal fistula treatment and recovery.
- Avoid using harsh chemicals: Chemicals in soaps, perfumes, and wipes can irritate the anal area, leading to further complications.
- Don’t skip follow-up appointments: Regular visits to your healthcare provider are essential for monitoring progress and detecting any potential issues early.
Why Our Non-Surgical Treatments Are the Right Choice for You
At Ayurcure, we understand the challenges that come with treating anal fistulas, and that’s why we’re here to guide you through your healing process with the best care possible. Our founder, Dr. S.K. Singh, is one of the most experienced fistula specialist doctors in Delhi, with over 30 years of expertise. With his extensive knowledge, he has helped countless patients overcome their anal fistula issues without the need for invasive surgery.
We believe that healing doesn’t always need to involve harsh procedures, which is why we focus on non-surgical treatments tailored to meet your unique needs. Under the expert guidance of Dr. S.K. Singh, we offer solutions like the Kshar Sutra treatment in Delhi, an Ayurvedic method designed to cleanse the fistula tract and promote natural healing.
As a leading provider of best fistula treatment in India, we ensure that each treatment plan is customized to ensure the fastest and most effective recovery possible.
- Faster recovery time with minimal downtime
- Reduced risk of complications compared to traditional surgery
- Personalized treatment plans tailored to individual needs
- Natural healing through Ayurvedic and non-invasive techniques
- No hospitalization required for most treatments
Book an appointment today to start your healing journey with Dr. S.K. Singh!
Conclusion
To summarize, healing an anal fistula requires proper care, the right treatment, and time. Non-surgical options like Kshar Sutra treatment and other Ayurvedic methods, such as fistula treatment in Ayurveda, can provide effective relief, reduce healing time, and prevent the need for invasive surgery. By following the right steps, such as maintaining hygiene, eating a fiber-rich diet, and getting enough rest, you can significantly speed up the recovery process. With over 30 years of experience, Dr. S.K. Singh offers the best fistula treatment in India, specializing in personalized non-surgical treatments that focus on faster recovery without surgery. Trust his expertise for a smoother, more comfortable healing journey.